Eligibility Verification
Reduce Denials and Costs, and Increase Operational Efficiency
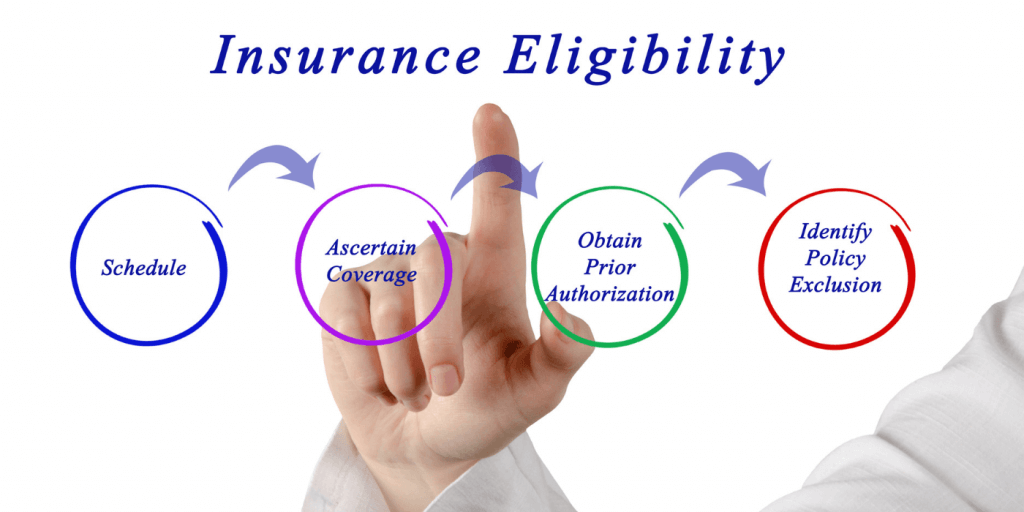
Claim denial is one of the major causes of disputes between patients and providers, and unfortunately this is often due to manual or filing errors caused by the lack of coverage information, or the improper verification of benefit information.
Usually, without e-verification, the patient would have to provide their insurance information before or at the time of their visit, at which point the provider would contact the payer to verify the information. The payer would then have to procure the correct information in a costly, time-consuming and error-prone process.
What inHealth’s eligibility verification solution offers you is not a simple eligibility and benefit verification solution, but a one-click operation in real-time using the National Identification Card, employing accurate and comprehensive technology, including all related coverage details such as deductibles, co-pay, top-up cards, along with dental and ophthalmological care to name a few.
Eligibility for payers
Eligibility for buyers
Eligibility for pharmacies
Features
Apply payer gatekeeping rules before rendering of service.
Seamless integration with all major electronic records (EHRs).
Use e-ID card to replace medical insurance card; complete transformation into e-platform.
Plan code matching to mitigate registration errors.
Insured members categorized under different statuses: “VIP, VVIP, etc…”
Solution tailored to your needs, which includes a mobile application, appointment module, pharmacies, and more.
Approve authorization for treatment from an appropriate source.
With OpenJet, inHealth’s eligibility verification allows healthcare providers to check patients’ coverage and benefits in real-time prior to their visit, thereby enhancing patient journey and experience. Patients also gain knowledge of their coverage details and can learn of charges not covered by their plans beforehand, eliminating distressing financial surprises. Payers, on the other hand, gain a reliable solution that manages the rising cost of internal operations and claims by eliminating manual errors.
In short, OpenJet’s Eligibility Verification enables a seamless workflow through real-time transactions driven from existing technology platforms. OpenJet provides you with real-time eligibility and benefits information to ensure that the appropriate payments are made and received.
Not only that, but it will also increase cost savings for both payers and providers by providing accurate eligibility benefit information at points of service and efficiently managing member data.
In case of referrals and prior authorizations, it can also manage them to achieve improved patient access among different network providers, while at the same time reducing medical and administrative costs.
Benefits

Replaces manual, time-consuming authorization process

Provide easy and direct API integration with customized endpoints
Save on administrative and operating costs
Real-time messaging between payers and providers

Alerts on excessive service use

Gatekeeping and care referral mechanisms

Increased revenue

Improved patient journey and satisfaction

Reduce technical denial claims through an automated check service

Increase provider revenue

Eliminate a major cause of payer-provider disputes
